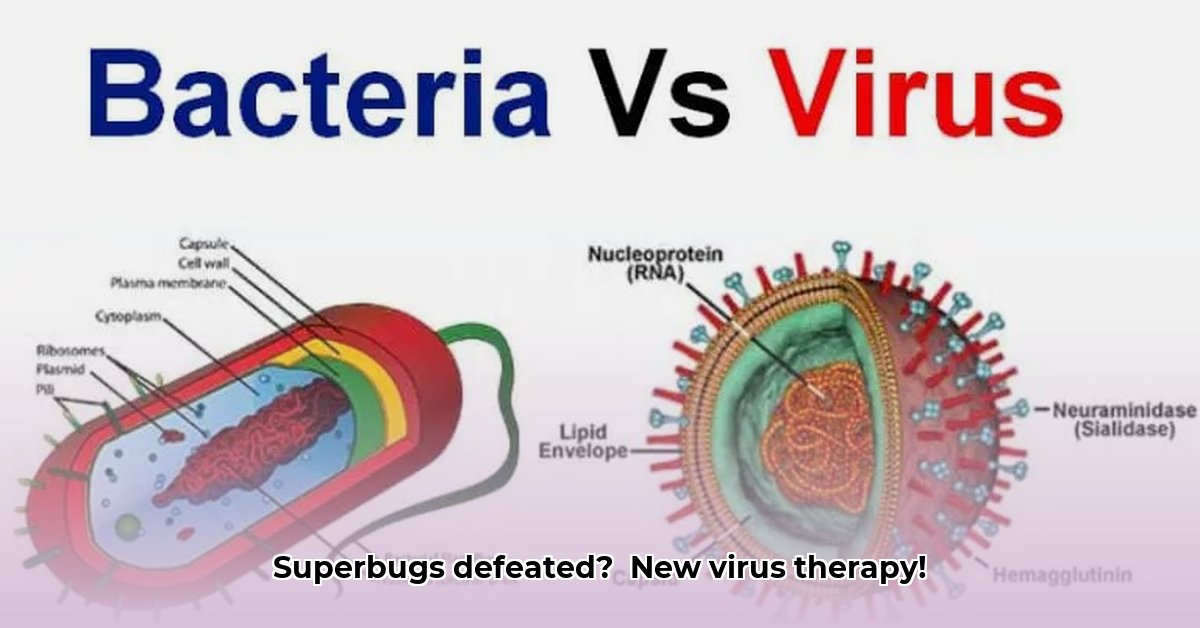
A Type of Virus That Infects Bacteria: Our Secret Weapon Against Superbugs?
Is there a way to effectively combat the ever-growing threat of superbugs – bacteria resistant to even our strongest antibiotics? The answer might lie in the microscopic world: bacteriophages (or simply "phages"), viruses that specifically target and destroy bacteria. These tiny natural predators have been battling bacteria for millennia, and now, scientists are harnessing their power to fight antibiotic-resistant infections. Think of them as nature's own targeted biological weapons – tiny, highly specific missiles designed to take out only the harmful invaders.
Understanding the Enemy: How Phages Work Their Magic
Phages employ diverse strategies to obliterate their bacterial foes. Two primary modes of action dominate: the lytic cycle and the lysogenic cycle.
The lytic cycle is a rapid, decisive attack. The phage attaches to a bacterium, injects its genetic material, commandeers the bacteria's cellular machinery to produce numerous copies of itself, and then, kaboom – the bacterial cell bursts open, releasing a swarm of new phages ready to repeat the process. It's a microscopic explosion of viral replication and bacterial destruction.
The lysogenic cycle is more subtle. The phage's genetic material integrates into the bacteria's DNA, becoming a silent passenger, sometimes remaining dormant for generations. However, under specific stressful conditions (like immune response or competition), the phage can switch back to the lytic cycle, launching a surprise attack. It's a bit like a sleeper agent, waiting for the perfect moment to strike. Yet another pathway, the pseudolysogenic cycle, adds another layer of complexity, often correlated to less-than-ideal conditions for the phage.
Aren't you amazed by the sheer ingenuity of these microscopic warriors? But how exactly can we utilise this natural phenomenon to our advantage?
Phage Therapy: A Blast from the Past, a Hope for the Future
The use of phages to combat bacterial infections is not a newfangled idea; in fact, it predates the widespread use of antibiotics. Early 20th-century scientists observed their effectiveness, but the discovery of antibiotics somewhat sidelined phage therapy. Now, with antibiotic resistance reaching crisis levels, the spotlight is back on phages. Why? Because their effectiveness against multiple drug resistant bacteria is undeniable.
The core principle is straightforward: identify the appropriate phage to target a specific infection-causing bacteria. But the reality is far from simple – finding the perfect match is a major challenge. We must ensure the phage is both effective and targeted whilst also considering its interaction with the body's own immune system. It's a complex dance between virus, bacteria, and human biology.
The Upsides and Downsides of Using Phages
Phage therapy boasts several significant advantages. Its high specificity is a major perk: unlike broad-spectrum antibiotics, which can decimate beneficial gut flora along with the harmful bacteria causing the infection, phages target only the disease-causing bacteria. Moreover, phages can evolve relatively quickly, potentially outpacing the development of resistance in the bacteria. This adaptability is a game-changer in the fight against superbugs.
However, significant challenges remain. Predicting a phage's effectiveness can be problematic; phages exhibit considerable variability, and their interplay with the immune system is complex. Improved methods for testing phage efficacy and safety are urgently needed. Large-scale phage production, while maintaining purity and safety, also presents a considerable hurdle.
Moving Forward with Phage Therapy: A Roadmap to Success
To fully realise the potential of phage therapy, a multifaceted approach is essential:
Standardization: Develop reliable methods for phage production, quality assurance, and efficacy testing, complemented by meticulously defined quality standards and efficient production facilities.
Rigorous Clinical Trials: Conduct large-scale, well-designed clinical trials to definitively establish the safety and efficacy of various phage combinations, particularly focusing initially on lytic phages for their predictable rapid-kill mechanisms.
Regulatory Frameworks: Establish clear guidelines and approval processes for phage therapies, ensuring safety, efficacy, and ethical considerations are integrated into the regulatory path.
Public and Professional Education: Educate both the public and healthcare professionals about phage therapy, clarifying its benefits, limitations, and safety profile to promote informed decision-making.
Collaborative Synergy: Promote collaborative efforts among researchers, pharmaceutical companies, regulatory bodies, and healthcare professionals to accelerate phage therapy development through enhanced research sharing, clinical data pooling, and combined expertise.
How to Predict Bacteriophage Therapy Efficacy Based on Phage Life Cycle
Predicting the success of bacteriophage therapy is crucial. A key factor is understanding the phage's life cycle, which directly influences its effectiveness as a therapeutic agent. The lytic cycle, with its rapid bacterial killing mechanism, is more predictable than the lysogenic cycle.
Key Factors Influencing Efficacy Predictions:
Phage Specificity: Does the phage only target the harmful bacteria, or does it also affect beneficial bacteria? Precise targeting is critical.
Lytic vs. Lysogenic: Lytic phages provide speed and predictability. Lysogenic phages, while potentially useful, introduce greater unpredictability.
Phage Concentration & MOI (Multiplicity of Infection): The ratio of phages to bacteria is crucial for effectiveness – higher MOI generally leads to more rapid bacterial killing.
Bacterial Burden: A higher bacterial load necessitates a larger phage dose for successful treatment.
Host Immune Response: The patient's immune system can influence the phage's activity and clearance.
In Vivo Conditions: The body's complex environment significantly impacts phage therapy efficacy.
Beyond these factors, sophisticated models, in vitro and in vivo testing, and the use of phage cocktails (combinations of multiple phages) hold the key to more accurate predictions and improved treatment success.
The future of phage therapy looks promising; however, sustained effort and careful research are critical to fully unleashing its potential. The fight against superbugs requires a multi-pronged strategy, and phage therapy, with its unique advantages, offers a valuable weapon in our arsenal.